Virtual Clinic Visit: Peripheral Vascular Case Study
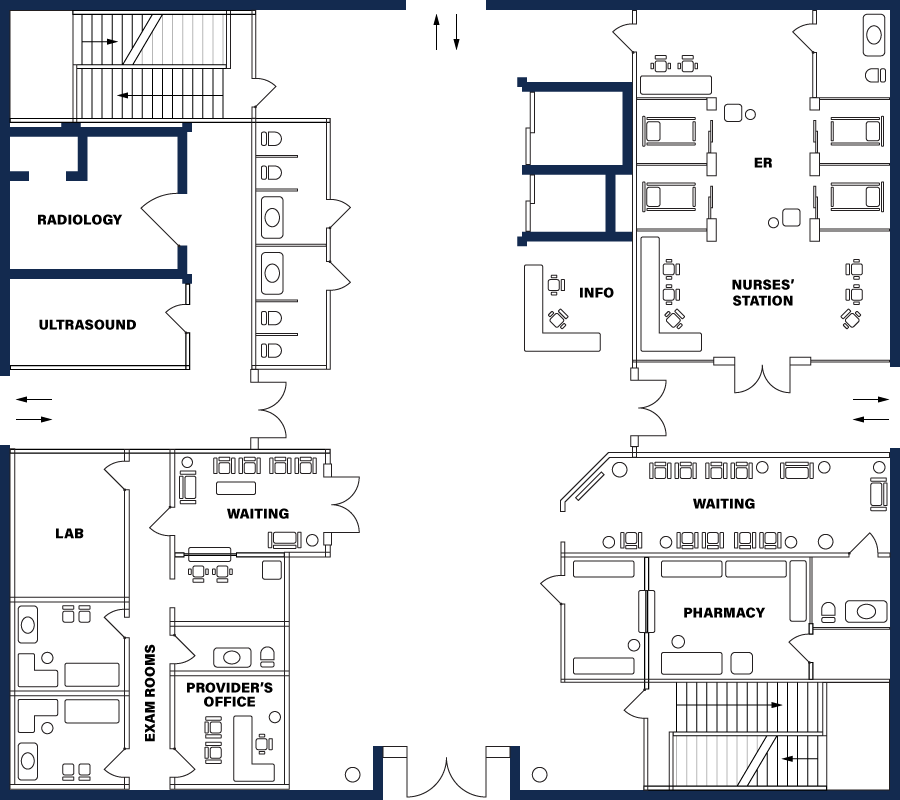
Introduction
Welcome to the Virtual Clinic! You will be visiting various rooms in the clinic collecting information and participating in activities that will lead you to a final summary. For each room that is available to visit, please make sure you complete the activity and use the information to make decisions for your patient. Please select the first available room you would like to visit from the Directory.



Nurse’s Station

Good morning, Pamela.

Good morning.

My name is Heather Williams, the nurse for Dr. Gleaton. I will need to take your vitals and gather additional health information prior to your appointment this morning. What is your concern today?

I have been having some dull aching chest pain that comes and goes over the past week, but it does get better once I rest.
Review Records
Full Name:
Pamela Penn
Gender:
Woman
Age:
52 years old
Address
181 Berkeley Ridge Dr. Lubbock, TX 29229
Height:
5’6"
Weight:
225 lbs. (BMI= 36.3 [obese])
Vital Signs:
Blood Pressure (BP): 132/90
Oxygen Saturation (O2): 100%
Pulse Rate (PR): 92
Respiratory Rate (RR): 18
Temperature: 98 degrees Fahrenheit
Personal History (PH)
Married for 30 years; 2 children (son 23 and daughter 25)
Family History:
Mother: 79, alive and well. Father: 54, deceased, heart attack. No siblings. There is a positive family history of hypertension, CAD, but no history of diabetes or cancers.
Social History:
Alcohol use: 1 or 2 beers each weekend; 5 glasses of wine once a week with dinner
Tobacco use: None
Medical History:
28 years old: Dx with hypertension and began taking an unknown betablocker. Stopped after 6 months because of drowsiness.
20 years old: Dx with peptic ulcer disease, which resolved after three months on cimetidine.
She always uses generic names; describes no history of cancer, lung disease, or previous heart disease.
Surgical History
Bunionectomy (28 years old); total abdominal hysterectomy (TAH) with bilateral salpingo-oophorectomy (BSO) 10 years ago.
Allergies:
Penicillin; experienced rash and hives in 1985
Immunization History:
Tdap (last received 15 years ago); Up to date with covid and flu vaccinations.
Medications Currently Taking:
HCTZ 12.5 mg; OTC Ibuprofen (Advil); multivitamin
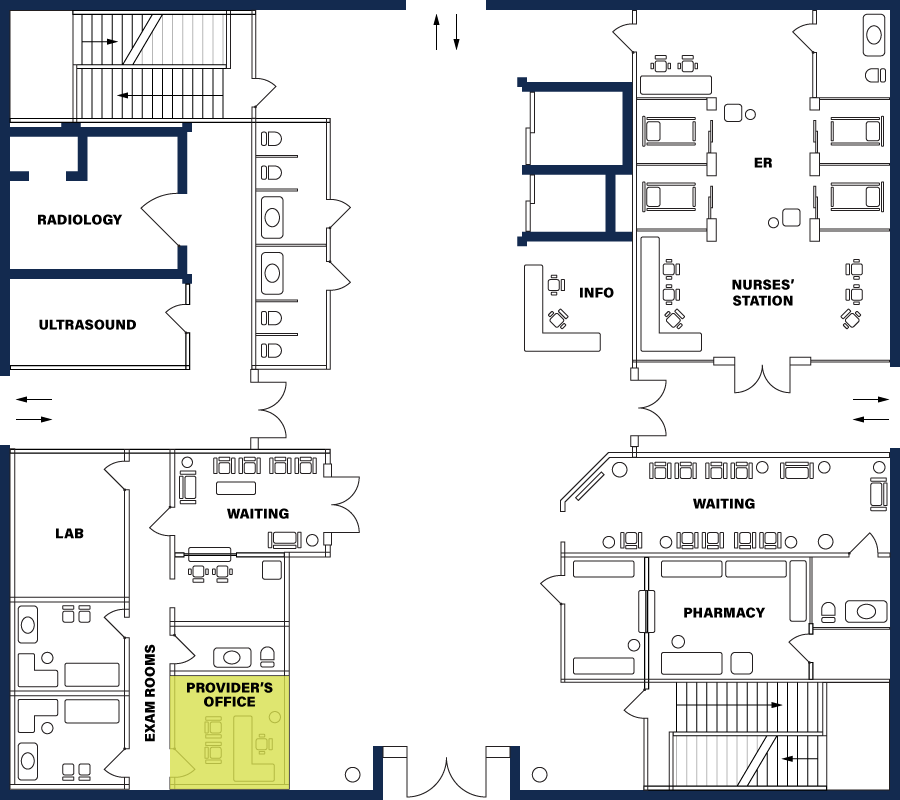
The Provider’s Office
Today, you see Pamela Penn, who is new to you, but an established patient at the clinic.

Good morning! I am Dr. Gleaton, one of the Nurse Practitioners here at the clinic. What do you prefer I call you and what brings you in today?

Good morning, Dr. Gleaton. You can call me Pamela. I am concerned about pain in my chest that I've noticed when I walk my dog.

Yes, this is concerning. Tell me more about this pain. Are you experiencing any symptoms right now?

No, I do not have any pain at this moment. My symptoms started about two weeks ago. I notice it when I work in my garden and walk my dog in the park. It always seems to be when I’m active. I thought it was just because I am overweight. I know I need to lose some weight and change my diet.

Tell me more about your pain. How long does it last? Does it resolve quickly?

Sometimes it would last from a few seconds to about a minute or so. It felt like a dull aching pain that started on my left side chest and arm. It starts during my walk and then goes away when I stop and rest.

How would you rate that pain on a scale of 1 to 10 with 10 being the worst pain?

Well, I would say the discomfort is about a 5/10.

Do you have any other symptoms? How about dizziness, heart palpitations, increased rate of breathing, shortness of breath, or trouble breathing when you try sleeping in a lying position? Do you ever have these symptoms when you are resting?

No, I don’t have any other symptoms that I can think of and I’ve never had the pain when I’m resting. Only when I walk and am more active. It’s hard because I know I need to lose some weight but it hurts when I walk, so what am I to do?

At this point have you tried anything to relieve your discomfort?

I have taken Ibuprofen 800 mg at least three times since experiencing my chest pain, I don’t know if it worked because the pain resolved so quickly after I rested. I also try to elevate my legs because my feet have started to get a little swollen if I’m on my feet a lot during the day.
Feedback
The patient is complaining of chest discomfort, which is the chief complaint. She also mentioned her feet swell at the end of the day and she is obese which you should be aware of and include in your medical note and decision making, but they are not the chief complaint.
Feedback
- Onset (Correct, 1-2 weeks)
- Location (Correct, left side of chest and arm)
- Duration (Correct, few seconds to 1 minute, resolve quickly with rest)
- Characteristic (Correct, dull ache)
- Aggravating factors (Correct, worsened when walking dog, gardening, walking)
- Relieving factors (Correct, relieved by rest, has tried ibuprofen as well)
- Timing (Correct, occurs with resolves quickly
- Severity (correct, 5/10 discomfort)
Feedback
Chest pain that occurs with activity and resolves quickly with rest is called stable angina. It is a symptom of coronary artery disease. Acute coronary syndrome is an acute cardiac event that would not present intermittently over weeks. Heart failure is high on the differential given her pain and the swelling in her feet. Costochondritis would present with different history and would be reproducible on examination. GERD is another consideration, it can also worsen with activity, but it would typically have heartburn symptoms, and symptoms when lying down.
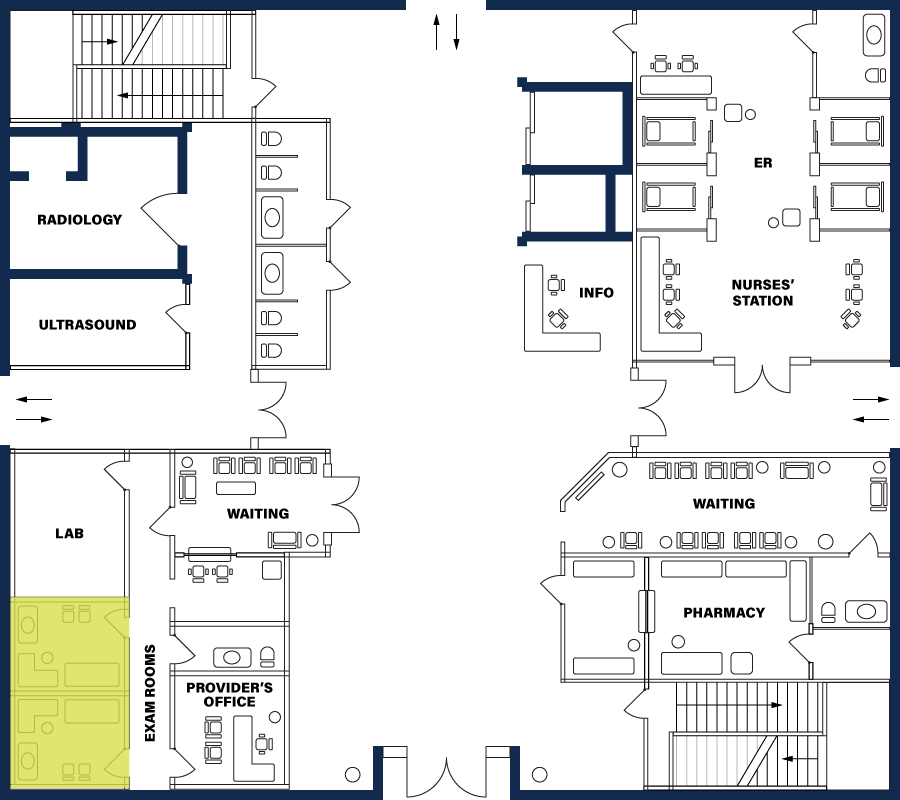
The Exam Room
Questions
Feedback
The NP should do a thorough cardiovascular examination. A peripheral vascular, and respiratory examination will be important to assess as well.
Exam Results:
General exam: obese ; CV: murmur or extra heart sound appreciated.
Heart rate is 96 on exam so it is difficult to distinguish the extra sound.
1+ pitting edema to bilateral lower extremities (BLE). Remainder of the exam is normal.

The Lab
Feedback
All of these labs should be ordered.
Dr. Gleaton ordered the following labs for Pamela:
- CBC (Complete Blood Count): can reveal fluid status, low oxygen levels in the blood due to lung or heart disease, tissue damage, infection
- Blood Urea Nitrogen (BUN): measures kidney function and amount of waste products in the blood. Pamela has hypertension and an elevated A1C which could be damaging to the kidneys.
- Creatinine: provides a value indicating the health of the kidneys; usually cleared by the kidneys, therefore an elevated level of creatinine could indicate poor kidney clearance because of the amount of waste product from the muscles are present.
- Electrolyte studies: can indicate hydration status
- Urinalysis: used to show possible proteinuria 24-hour urine collection—since the urinalysis does not provide the severity of proteinuria, a 24-hour urine collection test would further identify the cause of Pamela’s generalized edema.
- Cholesterol Levels: measures the amount of cholesterol in blood. Elevations indicate hyperlipidemia and can lead to atherosclerotic plaque buildup in the arteries.
- NT-proBNP: B-type natriuretic peptide (BNP) is a hormone produced by the heart. NT-proBNP is elevated in heart failure. Levels over 900pg/mL may indicate heart failure
- HgA1C is used to diagnose diabetes mellitus type 2.
View lab results
CBC (Complete Blood Count): Hemoglobin and Hematocrit [11.2 gram/100 ml; 30%] (low)
Blood Urea Nitrogen (BUN): [26 mg/dL] (high)
Creatinine: [1.1 mg/dL] (high)
Urinalysis: [+1 protein] (abnormal)
Cholesterol Levels: Total Cholesterol 288. HDL 30. LDL 226. Triglycerides 92
NT-proBNP: Results: 522pg/mL
HgbA1C: 6.2%
Radiology
Questions
Feedback
All of these tests and imaging can provide additional information. An echocardiogram uses ultrasound to view heart structures. It is useful to diagnose heart failure. Pharmacologic Stress test uses ECGs to record the heart's electrical pulses and evaluate blood flow to the heart. It is helpful to diagnosis ischemia and stable angina. An ECG can show changes suggestive of ischemia or infarction. A Coronary CT angiography uses computed tomography angiography to assess the coronary arteries and is useful in the diagnosis of coronary artery disease.
Feedback
ECGs are easily performed in the clinic, inexpensive and widely available. The other tests and imaging require special equipment.
The Provider's Office
You have successfully gathered the information needed to diagnose and treat the patient. The patient is back in the provider’s office to discuss next steps.
Questions
Feedback
The most likely cause of her symptoms, based on history and examination, is coronary artery disease causing stable angina.
Feedback
Pamela needs to be referred to cardiology for additional diagnostic testing and initiation of treatment.
Feedback
When you haven’t been able to establish a diagnosis for an encounter, code the condition or conditions to the highest degree of certainty, such as symptoms, signs, abnormal test results, or other reasons for the visit. You could also choose to address her obesity and prediabetes.
Feedback
At the beginning of the case study it was told to you that Pamela is an established patient at the clinic. Even though she is a new patient to you, since she has established care with another provider in the clinic, you need to use the established visit codes. Given the complexity of the visit, testing and consultation that needs to be ordered, a 99214 is the most appropriate code because the patient presents with an acute complicated problem requiring moderate medical decision making.
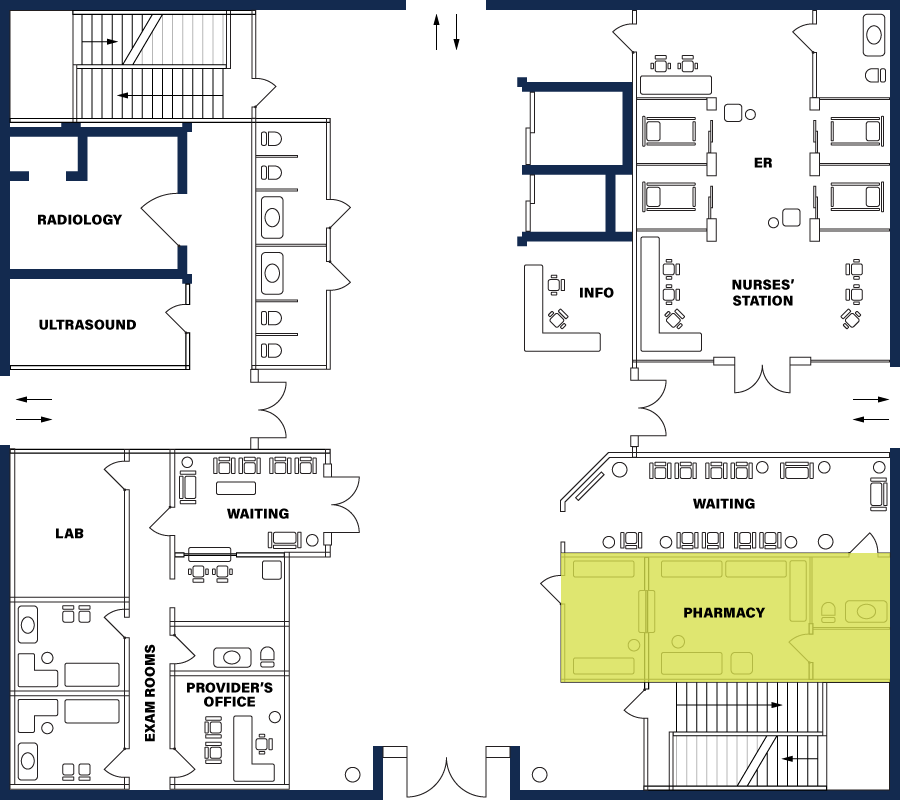
The Pharmacy
Question
Feedback
Patients with stable angina should be started on aspirin. This can safely be started prior to being seen by cardiology. Pamela should also be started on a statin medication due to her elevated LDL cholesterol levels and stable angina. She should be given a prescription for sublingual nitroglycerin with directions to take one every 5 minutes when required, up to 3 doses, even though her symptoms haven’t lasted longer than a minute. She will likely need beta-blocker and other antihypertensive medications, perhaps even antidiabetic medications that have cardiac protection effects.